- Schizophrenia affects 35 million adults worldwide each year
- First study to find that monoclonal antibody drug can provide symptom relief to people with schizophrenia and inflammation
- Randomised control trial
- Opens pathways towards personalised treatment of schizophrenia
Research conducted at Neuroscience Research Australia has found that an injection of an anti-flammatory biological known as Canakinumab in patients with schizophrenia and elevated inflammation brought about a decrease in psychotic symptom severity and inflammation. The research was published in Brain, Behavior, and Immunity.
“Our study is the first clinical trial of anti-inflammatories for people with schizophrenia who also have an elevated inflammation status,” says Professor Cyndi Shannon Weickert, lead author on the study and Senior Professor at Neuroscience Research Australia.
At the moment, all schizophrenia patients are treated with antipsychotic drugs. But the use of antipsychotic treatment shows limited improvement for cognitive and negative symptoms of schizophrenia.
“Our study shows that people with schizophrenia can lower their clinical signs of inflammation even one week after treatment with this monoclonal antibody, and this discovery opens up treatment options for people with schizophrenia beyond antipsychotics,”
Professor Weickert and collaborators’ study adds to a biological understanding of schizophrenia and signifies a new chapter in schizophrenia treatment that brings us closer to personalised options for individuals living with the disease.
The association between inflammation and schizophrenia
Growing evidence suggests an association between elevated levels of inflammation and psychiatric illness. However, studies prior to this one did not show any consistent or reproducible benefits in the use of anti-inflammatories for patients with schizophrenia.
“Prior studies investigated the benefit of anti-inflammatory drugs for people with schizophrenia regardless of their inflammation status,” says Professor Weickert. “Results of such prior studies were varied and inconsistent and any positive impacts of anti-inflammatory drugs were difficult to replicate.”
Professor Weickert’s study, however, took a new direction: it is the first study of anti-inflammatory drugs that exclusively recruited chronically ill schizophrenia patients with elevated peripheral blood markers of inflammation.
“Around 40% of people with chronic schizophrenia have inflammation,” says Professor Weickert. “Our approach in this study was unique to those conducted prior because we only expected anti-inflammatories to work for those people with schizophrenia who were experiencing inflammation.”
Professor Weickert attributes this targeted new approach as to why her team saw encouraging results.
Towards personalised treatment
Around 1% of Australians are affected by schizophrenia and 30% are considered treatment resistant. Schizophrenia greatly disrupts the lives of those affected and their friends and family, with around 80% of those diagnosed not being able to work.
The significance of the findings of Professor Weickert’s study is that it enhances biological understandings of schizophrenia and takes the field a step closer to personalised and more effective treatments for schizophrenia.
Current treatments for schizophrenia do not use a biological understanding of the illness.
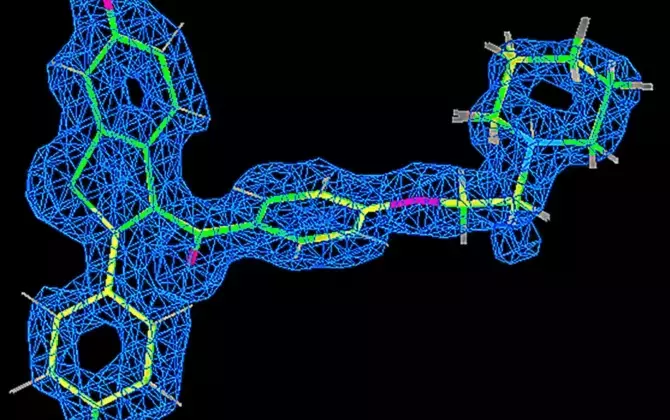
“Our research has focused biological and cellular changes in the brain and has provided us with two new directions in treatment of schizophrenia: one is to target the immune system and the other is hormone modulation,” says Professor Weickert.
This opens the possibility of a whole new classes of medication that is based on biological changes that are happening in the body and in the brain of people with schizophrenia.
“It’s exciting to discover that there are effective treatment options in addition to the stabilisation that anti-psychotics provide,” says Professor Weickert.
“Our results also suggest that schizophrenia has biological subtypes and that going forward, it will be important to select the right drug for the right person.”
Treating the body can help the brain
In psychiatry, all drugs work by having a direct effect on the brain.
“Everyone thinks that you’ve got to directly change what’s happening in the brain to see results in treatment of psychiatric illnesses,” says Professor Weickhert.
“But in our study, we saw benefit from a drug that’s working by affecting other parts of the body — in this instance the immune system — rather than directly modulating the brain.”
In the study, patients were already stabilised through an antipsychotic and were subsequently injected with one dose of Canakinumab. Results showed that when inflammation biomarkers went down because of the injection, psychotic symptoms such as hallucinations, hearing voices and paranoia subsequently decreased as well.
“We saw the largest reduction in inflammation at 4 weeks and psychotic symptoms at 8 weeks after injection compared to the placebo group,” says Professor Weickert.
“This shows that by blocking this one master regulator cytokine in the blood, then the brain may benefit.
“Meaning that what’s going on in the body is not separate from what’s going on in the brain, and in fact we think that understanding the brain-body connection is key to unlocking better treatments for people with schizophrenia.”